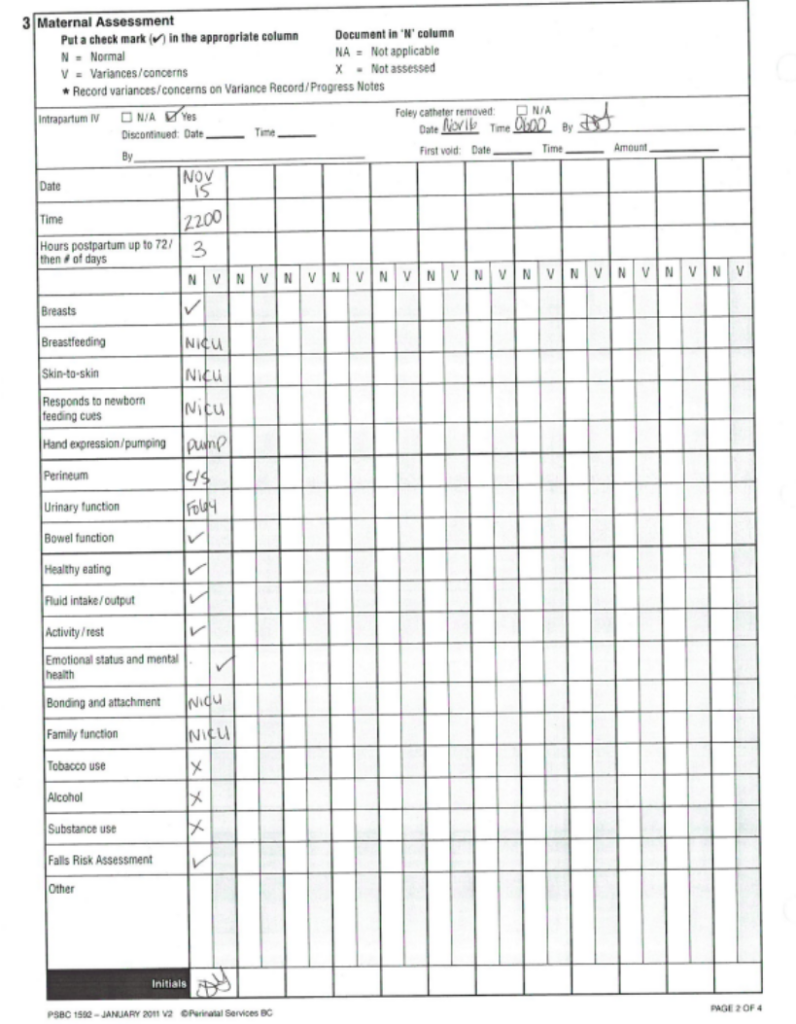
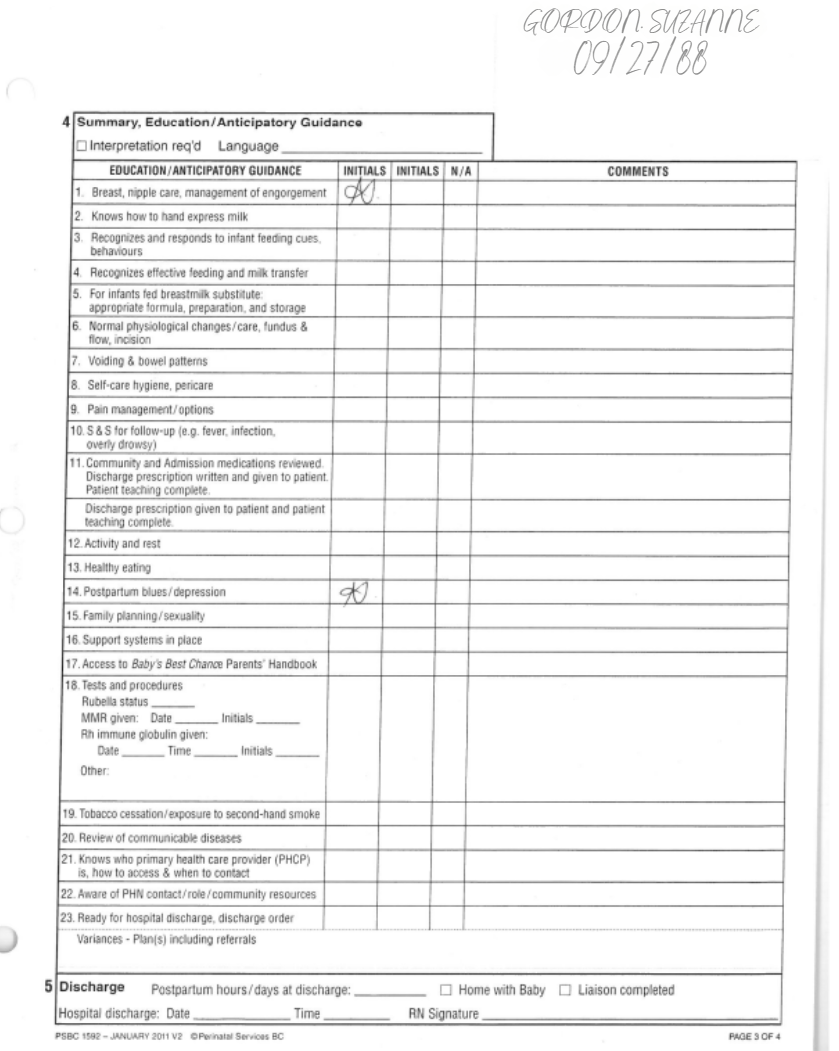
Patient Care Suzanne Gordon DOB 09/27/1988
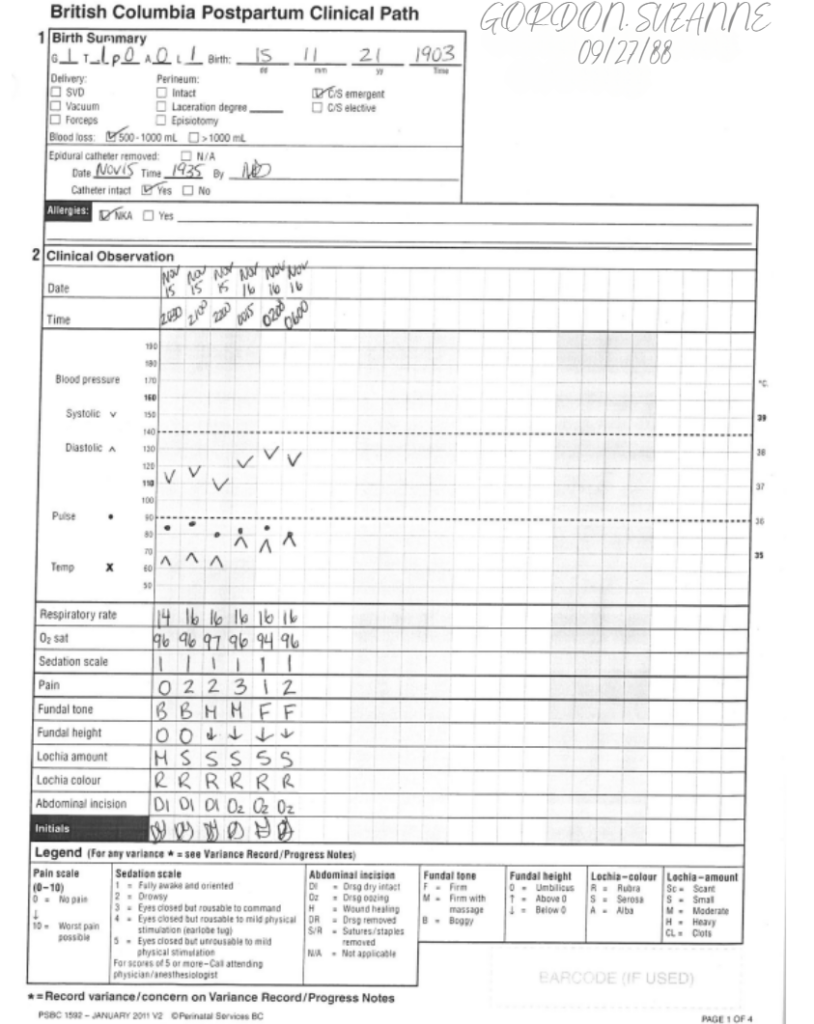
Vital Signs
| DAY | ||||||||
| TIME | ||||||||
| TEMPERATURE | ||||||||
| PULSE | ||||||||
| RESPIRATION | ||||||||
| BLOOD PRESSURE | ||||||||
| O2 SAT | ||||||||
| WEIGHT | ||||||||
| Initials | ||||||||
| DAY | ||||||||
| TIME | ||||||||
| TEMPERATURE | ||||||||
| PULSE | ||||||||
| RESPIRATION | ||||||||
| BLOOD PRESSURE | ||||||||
| O2 SAT | ||||||||
| Weight | ||||||||
| Initials | ||||||||
| DAY | ||||||||
| TIME | ||||||||
| TEMPERATURE | ||||||||
| PULSE | ||||||||
| RESPIRATION | ||||||||
| BLOOD PRESSURE | ||||||||
| O2 SAT | ||||||||
| Weight | ||||||||
| Initials | ||||||||
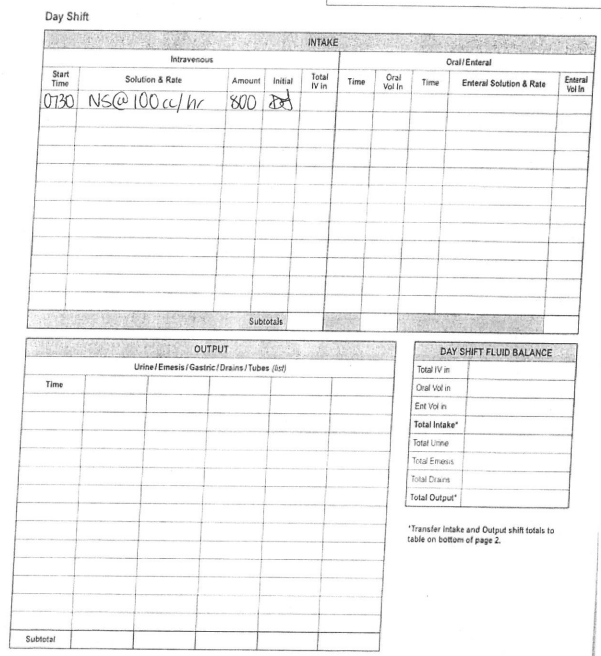
In/Out Record
Blood Glucose Record
| 0200 | Breakfast | Lunch | Dinner | HS | ||
| Date: Day of C/S | ||||||
| Time: | 1230 | 1700 | 2200 | |||
| Reading: | 5.6 | 9.8 | 8.7 | |||
| Comments: | ||||||
| Date: 1 day Post C/S | ||||||
| Time: | 0140 | 0800 | ||||
| Reading: | 6.0 | 9.2 | ||||
| Comments: | ||||||
| Wound Type/Etiology (if known) Pressure ☐ Venous ☐ Arterial ☐ Diabetic ☐ Surgical 2°Intent X Skin Tear ☐ Other ☐ | |||
| If Pressure Ulcer, chart stage: Stage 1_________ Stage 2_________ Stage3_________ Stage 4_________ Stage X(unstageable)_________ Stage SDTI (Suspected Deep Tissue Injury)_________ | |||
| MARK LOCATION OF WOUND/ULCER WITH AN ARROW OR AN ”X” | |||
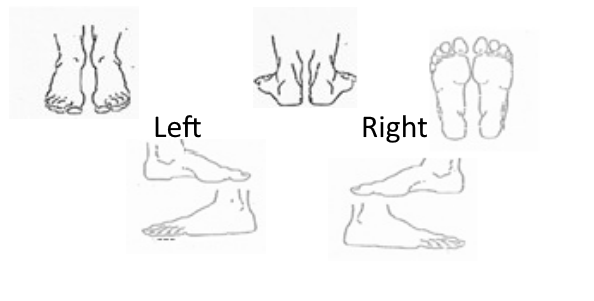 | 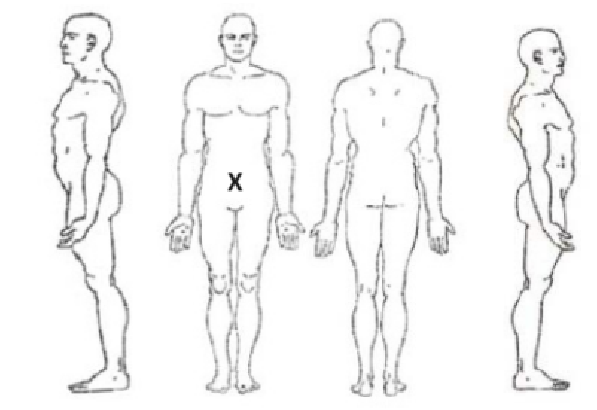 | 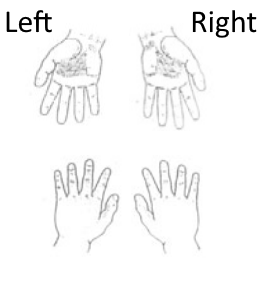 | |
| Legend: X or Blank Space = Not Applicable (as per agency) I * = Assessed/Completed I PN = See Progress Notes | |||
| Wound Location: RT hip (surgical site) | Date: surgical date | ||
| Time: | |||
Measurements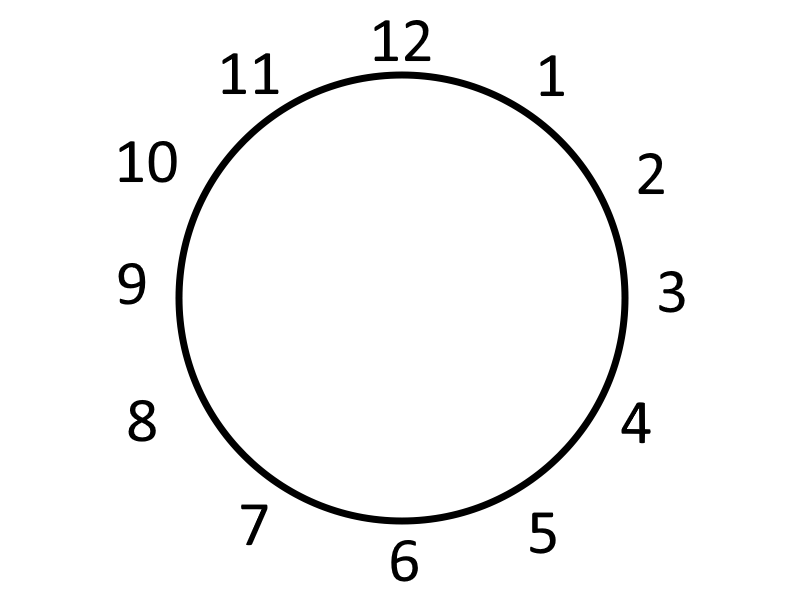 | Length | 5 cm | |
| Width | —- | ||
| Depth | —- | ||
| Sinus Tract #1 Depth | —- | ||
| Location (o’clock) | —- | ||
| Sinus Tract #2 Depth | —- | ||
| Location (o’clock) | —- | ||
| Undermining #1 Depth | —- | ||
| Location (o’clock) | —- | ||
| Undermining #2 Depth | —- | ||
| Location (o’clock) | —- | ||
| Wound Bed: Total % must = 100% | % Pink/Red | 100% | |
| % Granulation (red pebbly) | —- | ||
| % Slough | —- | ||
| % Eschar | —- | ||
| % Foreign body (sutures, mesh, hardware) | —- | ||
| % Underlying structures (fascia, tendon, bone) | —- | ||
| % Not visible | —- | ||
| % Other: | —- | ||
| Exudate Amount | None | —- | |
| Scant/small | YES | ||
| Moderate | —- | ||
| Large/copious | —- | ||
| Exudate Type | Serous | —- | |
| Sanguineous | YES | ||
| Purulent | —- | ||
| Other: | —- | ||
| Odor | Odour present after cleansing Yes or No | NO | |
| Wound Edge | Attached (flush w/ wound bed or ”sloping edge”) | YES | |
| Non-Attached (edge appears as a ”cliff”) | —- | ||
| Rolled (curled under) | —- | ||
| Epithelialization | —- | ||
| Peri-wound Skin | Intact | None | |
| Erythema (reddened) in cm | 2 cm | ||
| Indurated (firmness around wound) in cm | —- | ||
| Macerated (white, waterlogged) | —- | ||
| Excoriated/Denuded (superficial loss of tissue) | —- | ||
| Callused | —- | ||
| Fragile | YES | ||
| Other: | —- | ||
| Wound Pain (10 = worst) | Scored from 10 point analogue Pain Scale See Pain Assessment for details | 7/10 | |
| Treatment | If packing used, indicate # of packing pieces out/in | Out= _____ In=_____ | Out= _____ In=_____ |
| Treatment Plan Cleanse with normal saline, dry, apply abd pad, change 5 days post op. | |||
| Date Initiated: | 5 days post op | ||
| Plan: remove staples 7 days after surgery, ensure well approximated wound edges, apply steri-strips | |||
| Date D/C: | |||
| Date Initiated: | |||
| Plan: | |||